Facial Nerve

Slide

Slide
Facial Nerve
Anatomy and Function of the Facial Nerve
The facial nerve, also called cranial nerve VII, is one of the twelve cranial nerves that come directly from the brain. It starts in the brainstem and travels through the skull to reach the face. Along its path, the nerve branches out into smaller nerves that control different parts of the face. These branches are responsible for moving the muscles of facial expression, like smiling, frowning, or closing the eyes. The facial nerve also carries signals to some glands, such as the salivary and tear glands, and helps with taste on the front two-thirds of the tongue (Standring, 2021). .
The main job of the facial nerve is to control facial movements and expressions, but it also has sensory and secretory functions. It helps us show emotions through our face, taste sweet and salty flavors, and even keep our eyes moist by stimulating tear production. Because the facial nerve has many roles, damage to it can cause weakness or paralysis on one side of the face, loss of taste, or dryness in the eyes and mouth (Brazis, Masdeu, & Biller, 2012).
The main job of the facial nerve is to control facial movements and expressions, but it also has sensory and secretory functions. It helps us show emotions through our face, taste sweet and salty flavors, and even keep our eyes moist by stimulating tear production. Because the facial nerve has many roles, damage to it can cause weakness or paralysis on one side of the face, loss of taste, or dryness in the eyes and mouth (Brazis, Masdeu, & Biller, 2012).
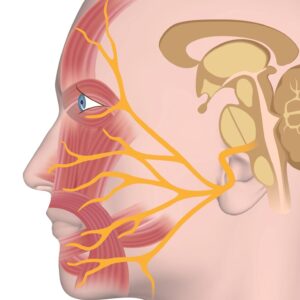
The Facial Nerve comes directly from the brain and has a complex structure in the face.
Dr. Yver discusses the facial nerve and its function
FLACCID FACIAL PARALYSIS
Up to 60% of facial paralysis patients meet clinical criteria for depression and/or anxiety disorder. Several studies have found that observers perceive facial paralysis patients as more distressed, less trustworthy, and less intelligent. When casual observers interact with facial paralysis patients, they frequently misinterpret facial expressions, leads to a negative expression for both parties. A study in JAMA Facial Plastic Surgery quantified the health utility scores of various health states, and found that unilateral facial paralysis ranked worse than monocular blindness
Dr. Yver describes the emotional impact of facial paralysis on pateints.
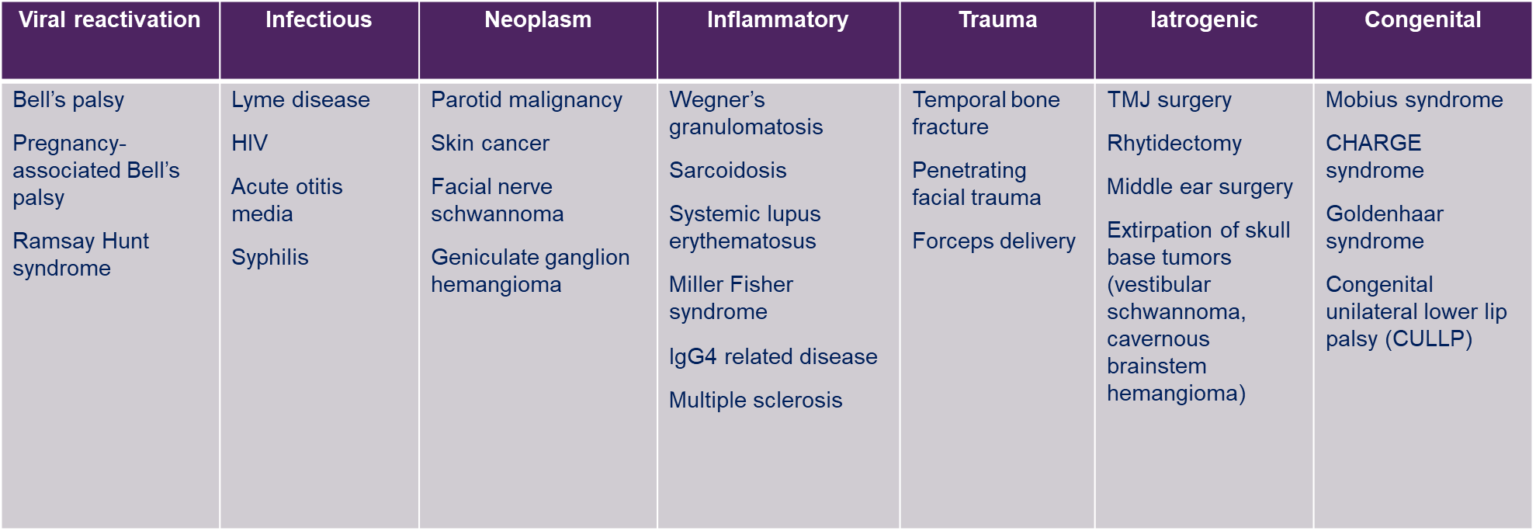
Causes of Facial Paralysis
There are many causes of facial paralysis ranging from viral infections to congenital factors. Review the table below and list to Dr. Yver describe these various causes.
Dr. Yver describes the many causes of facial paralysis.
Viral Reactivation Facial Paralysis
Multiple viral reactivation can cause facial paralysis. These include:
- Bell’s palsy (HSV) and Ramsay Hunt syndrome (VZV) account for up to 70% of acute facial paralysis
- Characterized by acute onset (within 24 hours), complete facial paralysis
- Ramsay Hunt Syndrome (RHS) is also characterized by CN VIII involvement (hearing loss and/or vertigo) +/- a vesicular rash.
These reactivations can be treated medically with steroids and antivirals and spontaneous recovery is typically observed within 4-6 months.
Viral reactivation account for most of acute facial paralysis cases
Flaccid Facial Paralysis: Current Treatment Paradigm
Dr. Yver describes treatment options for flaccid facial paralysis.
Treatment of the Brow-Lid Complex
- Prioritize corneal protection and lubrication; referral to ophthalmology if needed
- Placement of a thin-profile upper eyelid weight – helps with eye closure
- Lower lid tightening for patients with significant lower lid laxity of ectropion (typically older patients)
- Brow lift – can improve facial symmetry and improve ocular hygiene
Static Suspension Techniques
- Typically, 4-5 bands inset: NLF (most important), nasal valve, philtrum, oral commissure, +/- lower lip.
- Suture suspension technique can be a less invasive alternative.
Dynamic Reinnervation: Cross-facial nerve graft
- A donor branch from the contralateral (unaffected side) is hooked up to a sural nerve graft, which is routed across the face to the paralyzed side.
- Anecdotally, we have had good success with CFNG
o To power gracilis
o To augment the smile in partial facial paralysis
o To augment lower lip function
Dynamic Reinnervation: Cross-facial nerve graft
- Gracilis free muscle transfer is the gold standard for dynamic reinnervation outside of the 24-month window
- The gracilis muscle is harvested from the medial thigh along with its vascular pedicle and the anterior obturator nerve
- Often performed in combination with fascia lata
- Neurotization source:o Masseteric nerve
o Cross facial nerve graft
o Dual innervated
o Ipsilateral facial nerve twig
If you are suffering from compression symptoms, be sure to consult a nerve specialist
SYNKINESIS
Flaccid paralysis and synkinesis are both conditions that affect muscle movement, but they have opposite effects. Flaccid paralysis occurs when muscles become weak or completely lose their ability to move due to nerve damage. This happens because the connection between the brain and the muscles is disrupted, leading to limp and unresponsive muscles. In contrast, synkinesis happens when movements that should be separate occur together unintentionally. This usually occurs after nerve damage heals incorrectly, causing the wrong signals to reach the muscles. For example, someone recovering from facial nerve damage might experience eye closure when trying to smile. While flaccid paralysis results in a lack of movement, synkinesis causes excessive or misdirected movement, showing how nerve damage can affect the body in different ways.
Dr. Yver discusses the difference between synkinesis and paralysis.
- Synkinesis can occur after transient injury to the facial nerve, such as after Bell’s palsy.
- It is characterized by muscle tightness, facial asymmetry, disorganized muscle movements, and inability to make normal facial expressions.
- Described as a “frozen” face.
Treatment of Synkinesis
Physcial Therapy
- Ideally performed by a licensed physical therapist with specialized training in facial nerve disorders
- Facial rehabilitation for synkinesis includes 5 main components:
1) patient education,
2) soft tissue mobilization to address the muscle tightness/contracture,
3) functional retraining to improve oral competence,
4) facial expression retraining using neuromuscular retraining, and
5) synkinesis management - Emphasis on self-management techniques and education
Botox Therapy
- Administered every 3-4 months
- Goal is to balance the face, address muscle spasm/pulling, and improve functional issues (e.g. dysarthria and oral incompetence)
- Through insurance!
Selective Neurectomy
- Depressor anguli oris resection (“smile release” procedure) — intra-oral exposure and resection of the DAO muscle alleviates downward drag on the oral commissure to release the smile
- Safe and well tolerated; performed in the clinic setting
- Excellent adjunct to Botox
Dr. Yver discusses treatment options for facial synkinesis.
PAGE CONTRIBUTORS
PAGE CONTRIBUTORS


Christina Yver, MD
Facial Plastic & Reconstructive Surgery
University of Pittsburgh Medical Center


Matthew Spector, MD
Head and Neck Surgeon
University of Pittsburgh
Medical Center
The content on or accessible through globalnervefoundation.org is for informational purposes only. This information is not a substitute for professional advice or expert medical services from a qualified healthcare provider
